Recovering with Post Prostatectomy Physical Therapy
Post Prostatectomy Pelvic Floor Physical Therapy Benefits
Introduction Prostate cancer is the most common type of cancer in men older than 50. Survival rates for prostate cancer are increasing thanks to early detection through PSA testing and advancements in surgical techniques and treatments, such as a prostatectomy. However, a prostatectomy can negatively affect your pelvic health, resulting in incontinence or erectile dysfunction. Pelvic floor physical therapy can address issues related to your pelvic floor muscle impairments and significantly improve your quality of life post-surgery.
Pelvic Floor Physical Therapy for Prostatectomy
When cancer is detected in the prostate, the benefits of a prostatectomy are unquestionable. It is a life-saving procedure to remove cancer from your body, but it also comes with risks and complications such as:
Erectile dysfunction
Sterility
Lymphedema
The most significant complaints after surgery are urinary incontinence and erectile dysfunction, which negatively affect both quality of life and social interactions. While symptoms usually improve on their own over time, at least 8% of men continue to live with complications up to two years following surgery.
Often, men in the U.S. are not instructed to see a physical therapist until they attempt Kegel exercises (contracting pelvic floor muscles) on their own for several months after prostate surgery. However, seeking physical therapy sooner can improve pelvic floor function and relieve urinary incontinence and erectile dysfunction more effectively.
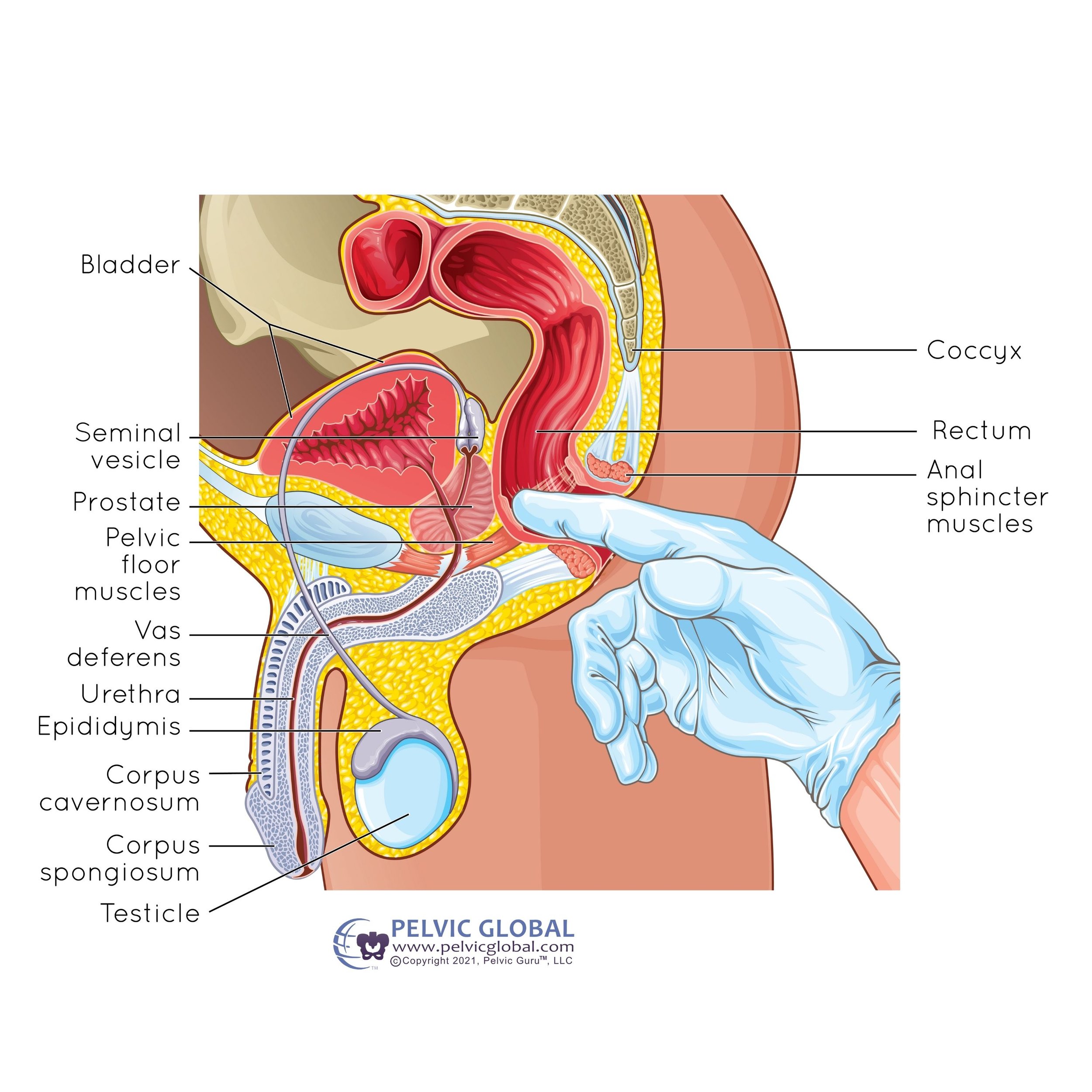
Key Components of the Male Pelvic Floor
Bladder: The bladder is the organ that stores urine. It is located above the prostate.
Seminal Vesicle: These are glands that secrete fluid that partly composes semen.
Prostate: A walnut-sized gland located below the bladder. It surrounds the urethra and contributes to seminal fluid.
Pelvic Floor Muscles: These muscles support pelvic organs, control continence, and play a role in sexual function.
Vas Deferens: The duct that transports sperm from the testicle to the urethra.
Urethra: The tube that carries urine from the bladder to the outside of the body. In men, it also carries semen during ejaculation.
Epididymis: A tube that stores and carries sperm.
Corpus Cavernosum: Erectile tissue that fills with blood to produce an erection.
Corpus Spongiosum: Erectile tissue that surrounds the urethra and prevents it from being pinched closed during erection.
Testicle: The organ that produces sperm and testosterone.
Coccyx: The tailbone, located at the bottom of the spine.
Rectum: The final section of the large intestine, terminating at the anus.
Anal Sphincter Muscles: Muscles that control the expulsion of feces from the rectum.
The Prostate’s Focus
The prostate is a vital gland in the male reproductive system. It surrounds the urethra just below the bladder and plays a crucial role in the production of seminal fluid, which nourishes and transports sperm.
Key Functions of the Prostate:
Producing seminal fluid that mixes with sperm to form semen.
Enhancing sperm motility and viability.
Helping to expel semen during ejaculation through muscle contractions.
Benefits of Early Physical Therapy Intervention
Pelvic floor muscle training is the first line of defense for complications related to post-prostatectomy. Physical therapy offers the following treatments to help you quickly reach your goals:
Therapeutic Exercise: Tailored exercises to strengthen pelvic floor muscles.
Electrical Stimulation: Helps stimulate muscle contractions and improve strength.
Biofeedback Therapy: Provides visual, auditory, or tactile feedback to help you understand and improve muscle control.
Bladder Training: Techniques such as timed voiding or urge suppression can help to improve bladder control and reduce incontinence.
Education and training of your pelvic floor muscles are essential to achieving a properly functioning pelvic floor. You can start your training before and after surgery. Training for specific functions, such as continence or erection, must include exercises that resemble the desired actions.
Pelvic Floor Exercises After Prostatectomy
Urinary incontinence is common following radical prostatectomy. There are several types of incontinence due to a poorly functioning pelvic floor:
Stress Incontinence: Occurs when urine leaks due to increased abdominal pressure, such as during a sneeze, cough, or lifting something heavy.
Urge Incontinence: This is urinary leakage when you feel the need to urinate.
Mixed Incontinence: When you experience both stress and urge incontinence, making it difficult to manage with strengthening exercises alone.
Strengthening your pelvic floor muscles will help you control your urge to urinate and hold back urine until you are ready to relieve yourself. The pelvic floor muscles are responsible for:
Bladder stability
Resting urethral pressure
Regulation of urethral pressure during exertion
Erection and maintaining erection
Training your pelvic floor muscles can prevent urine from leaking accidentally and increase the rigidity of your erections.
What to Expect from Physical Therapy After Prostate Surgery
Our physical therapists can address your pelvic floor muscles and design an exercise program specific to the actions you want to complete, such as maintaining continence during physical activity and sexual performance.
First, an examination will be done to determine the strength, symmetry, and tone of your pelvic floor muscles. This includes palpating or touching your anorectal tissues, urogential muscles, and perineal body. The therapist will observe your anal contraction and penis lift. You may also need to complete a voiding diary and questionnaires regarding your symptoms to give your physical therapist a complete picture of your situation.
Once the therapist collects enough information, they can develop a diagnosis and create an individualized pelvic floor muscle training program to help you reach your goals.
Your individualized program may include:
Therapeutic Exercises: To improve strength and coordination of pelvic floor muscles. These exercises go beyond kegels because considering the rest of your body with your pelvic floor is crucial.
Stretching and Breathing Exercises: To promote relaxation and full proper function of your pelvic floor is important, especially in times of stress incontinence.
Lifestyle Modifications: Education on habits and activities that support pelvic health.
Important Muscles for Pelvic Floor Synergy
Weak synergy, or unbalanced activation between your pelvic floor muscles and other core muscles, is believed to contribute to pelvic floor dysfunction. Important muscles to address include:
Transversus Abdominis: Stomach muscles
Gluteus Maximus: Butt muscles
Adductor Femoris: Inner thigh muscles
Direct local trauma from radical prostatectomy can result in deficiencies in muscle recruitment, whether you are experiencing pain or not.
Top 10 Tips for Post Prostatectomy Physical Therapy
Start Early: Begin pelvic floor exercises as soon as possible, this means even before surgery.
Stay Consistent: Regular exercise is key to improvement.
Use Biofeedback: Helps improve muscle control and coordination, and remember this goes beyond biofeedback with a machine.
Include Core Exercises: Strengthen related muscle groups for better synergy.
Monitor Progress: Keep a diary of your symptoms and improvements.
Stay Hydrated: Proper hydration supports overall bladder health, despite common misconceptions that drinking less will cause less leakage.
Practice Relaxation: Stress management can improve muscle function because when your are stressed your pelvic floor muscles are one of the first to go into spasm.
Avoid Heavy Lifting: Specifically heavy lifting or difficulty tasks while holding your breath. This can cause stress incontinence.
Seek Professional Guidance: Work with a certified pelvic floor physical therapist.
Stay Positive: Patience and persistence are crucial for recovery.
FAQs about Post Prostatectomy Physical Therapy
Q: How soon after surgery can I start physical therapy? A: It's best to start pelvic floor exercises as soon as your doctor gives the okay, often within a few weeks post-surgery.
Q: How long does it take to see improvement? A: While some men see improvements within a few weeks, it can take several months of consistent exercise to achieve significant results.
Q: Can physical therapy help with erectile dysfunction after prostate surgery? A: Yes, pelvic floor exercises can improve muscle strength and coordination, which can help with erectile dysfunction.
Q: Is it ever too late to start physical therapy after prostate surgery? A: No, it’s never too late to start. Physical therapy can be beneficial at any stage post-surgery.
Conclusion Pelvic floor physical therapy is a critical component of recovery after prostatectomy. By starting therapy early and staying consistent, you can significantly improve urinary incontinence and erectile dysfunction, enhancing your overall quality of life. Don't hesitate to seek professional guidance to ensure you're on the right path to recovery.
Written by:
Dr. Jana Richardson, PT, DPT, WCS, PRPC, CIDN
Dual Board Certified Pelvic Floor Therapist and Owner of Chicago Pelvic Health
Dr. Jana Richardson is a highly accomplished pelvic floor therapist with dual board certifications and extensive experience in treating complex pelvic floor dysfunctions. As the owner of Chicago Pelvic Health, Dr. Richardson is dedicated to providing personalized and effective care for her patients. With a Doctorate in Physical Therapy, and specialized certifications in Women’s Health and Pelvic Rehabilitation, Dr. Richardson is a leading expert in her field. She is also certified in Integrative Dry Needling, further enhancing her ability to offer comprehensive treatment plans. Dr. Richardson’s commitment to patient-centered care and her passion for helping individuals achieve optimal pelvic health make her an invaluable asset to the community.
Contact Information