Managing Chronic Prostatitis with Pelvic Floor Physical Therapy: A Proven Approach to Relief
Chronic prostatitis is a common yet often misunderstood condition affecting many men worldwide. This blog aims to shed light on how pelvic floor physical therapy (PT) can be the best treatment option for chronic prostatitis, helping men manage symptoms and improve their quality of life.
Understanding Chronic Prostatitis
Chronic prostatitis, also known as chronic pelvic pain syndrome (CPPS), is characterized by persistent pelvic pain and urinary symptoms. It accounts for about 90% of prostatitis cases and is not typically caused by bacterial infections. There are four categories of prostatitis:
Category I: Acute Bacterial Prostatitis
An acute infection of the urinary tract.
Category II: Chronic Bacterial Prostatitis
Recurrent infection of the prostate.
Category III: Chronic Prostatitis / Chronic Pelvic Pain Syndrome (CPPS)
May or may not occur with inflammation. Antibiotics typically do not help with this diagnosis.
Category IV: Asymptomatic Prostatitis
Higher levels of white blood cells with no genitourinary symptoms.
Categories I and II are due to bacterial infections and are treated with antibiotics. Category IV usually does not require treatment. However, Category III, which is most common, involves myofascial and neurological issues that benefit from pelvic floor physical therapy.
Chronic prostatitis, also known as chronic pelvic pain syndrome (CP/CPPS), involves persistent pain in the area of the prostate gland. CP/CPPS is the most common form of prostatitis.
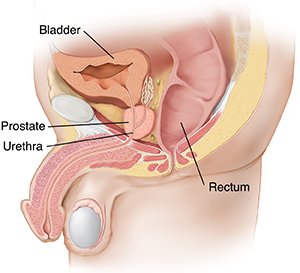
The prostate gland, a crucial part of the male reproductive system, is located just below the bladder and surrounds the urethra. The urethra is the tube that carries urine and semen out of the body. Symptoms like pain and difficulty urinating may vary in intensity and frequency.
Symptoms of Chronic Prostatitis
Chronic prostatitis can cause a variety of symptoms, including:
Bladder Symptoms: Urgency, frequency, hesitancy, changes in stream, or pain during urination.
Bowel Symptoms: Constipation, difficulty emptying bowels, or pain before/during/after bowel movements.
Sexual Dysfunction: Erectile dysfunction, pain with arousal/intercourse, and pain with ejaculation.
Genital Pain: Testicular or penile pain/discomfort.
Anal/Rectal Pain: Feeling of “golf ball in rectum” or “sitting on a rock.”
Musculoskeletal Pain: Hip pain, groin pain, tailbone pain, abdominal pain, or low back pain.
The Role of the Pelvic Floor in Men
The male pelvic floor muscles support the bladder, prostate, bowel, and other pelvic organs. They allow for proper urination, defecation, and sexual intercourse. These muscles can develop dysfunctions such as spasms, tightness, weakness, and impaired coordination, leading to the symptoms mentioned above.
Pelvic Floor Physical Therapy for Chronic Prostatitis
Pelvic floor physical therapy is a specialized form of therapy that focuses on the muscles, tissues, and nerves of the pelvic floor. A trained pelvic floor physical therapist can help reduce symptoms and restore normal functioning. Here's how:
Initial Evaluation: The first visit involves a detailed evaluation to determine the cause and contributing factors to each patient's complaints. The therapist will discuss the findings and develop a personalized plan of care.
Home Program: The therapist will provide an individualized home program consisting of exercises, stretches, and behavioral modifications.
Follow-up Visits: These visits may include various therapy techniques such as:
Myofascial Release
Coordination Exercises/Training
Therapeutic Exercise
Manual Therapy
Relaxation Exercises
Behavioral Recommendations
Postural Education/Training
Biofeedback
Modalities (e.g., e-stim, TENS, ultrasound)
FAQs About Chronic Prostatitis and Pelvic Floor PT
What are the common symptoms of chronic prostatitis?
Symptoms include pelvic pain, urinary issues, sexual dysfunction, and musculoskeletal pain.
How is chronic prostatitis diagnosed?
Diagnosis typically involves ruling out bacterial infections and identifying symptoms that persist for at least three months.
Can pelvic floor physical therapy help with chronic prostatitis?
Yes, pelvic floor physical therapy can alleviate symptoms by addressing muscle dysfunction and improving pelvic floor health.
What should I expect during a pelvic floor PT session?
Expect a detailed evaluation, personalized treatment plan, and various therapy techniques aimed at reducing symptoms and restoring function.
How long does it take to see improvements with pelvic floor PT?
Improvement timelines vary, but many patients notice significant symptom relief within a few weeks to months of consistent therapy.
Similar Pelvic Floor Dysfunctions Related to Chronic Prostatitis
Chronic prostatitis can lead to or coexist with other pelvic floor dysfunctions, including:
Chronic Pelvic Pain Syndrome (CPPS)
Erectile Dysfunction
Painful Bladder Syndrome/Interstitial Cystitis
Coccygodynia (tailbone pain)
Conclusion
Pelvic floor physical therapy offers a promising treatment option for men suffering from chronic prostatitis. By addressing the underlying muscle dysfunction and providing personalized care, pelvic floor PT can help alleviate symptoms and improve quality of life. If you or someone you know is experiencing symptoms of chronic prostatitis, consider consulting a pelvic floor physical therapist to explore this effective treatment option.
Written by:
Dr. Jana Richardson, PT, DPT, WCS, PRPC, CIDN
Dual Board Certified Pelvic Floor Therapist and Owner of Chicago Pelvic Health
Dr. Jana Richardson is a highly accomplished pelvic floor therapist with dual board certifications and extensive experience in treating complex pelvic floor dysfunctions. As the owner of Chicago Pelvic Health, Dr. Richardson is dedicated to providing personalized and effective care for her patients. With a Doctorate in Physical Therapy, and specialized certifications in Women’s Health and Pelvic Rehabilitation, Dr. Richardson is a leading expert in her field. She is also certified in Integrative Dry Needling, further enhancing her ability to offer comprehensive treatment plans. Dr. Richardson’s commitment to patient-centered care and her passion for helping individuals achieve optimal pelvic health make her an invaluable asset to the community.
Contact Information