Treating Pudendal Neuralgia in Men and Women: The Role of Pelvic Floor Physical Therapy
Understanding Pudendal Neuralgia in Men and Women
Pudendal neuralgia is a condition that can cause significant pain and discomfort in the pelvic region for both men and women. This pelvic health blog will explore how pelvic floor physical therapy (PT) can effectively treat pudendal neuralgia, providing physical and emotional relief in an area where patients often feel like they are sprinning their wheels.
What is Pudendal Neuralgia?
Pudendal neuralgia is a condition where the pudendal nerve is irritated, leading to pain or discomfort in the pelvic region, often resulting in chronic pelvic pain. Nerves get irritated either through a direct injury, compression, being stretched or pulled on, or entrapment. Since nerves don’t like to get stuck, it results in symptoms like stabbing, burning, or shooting pain that can be felt in the buttocks, perineum, and genital area, often worsening when sitting.
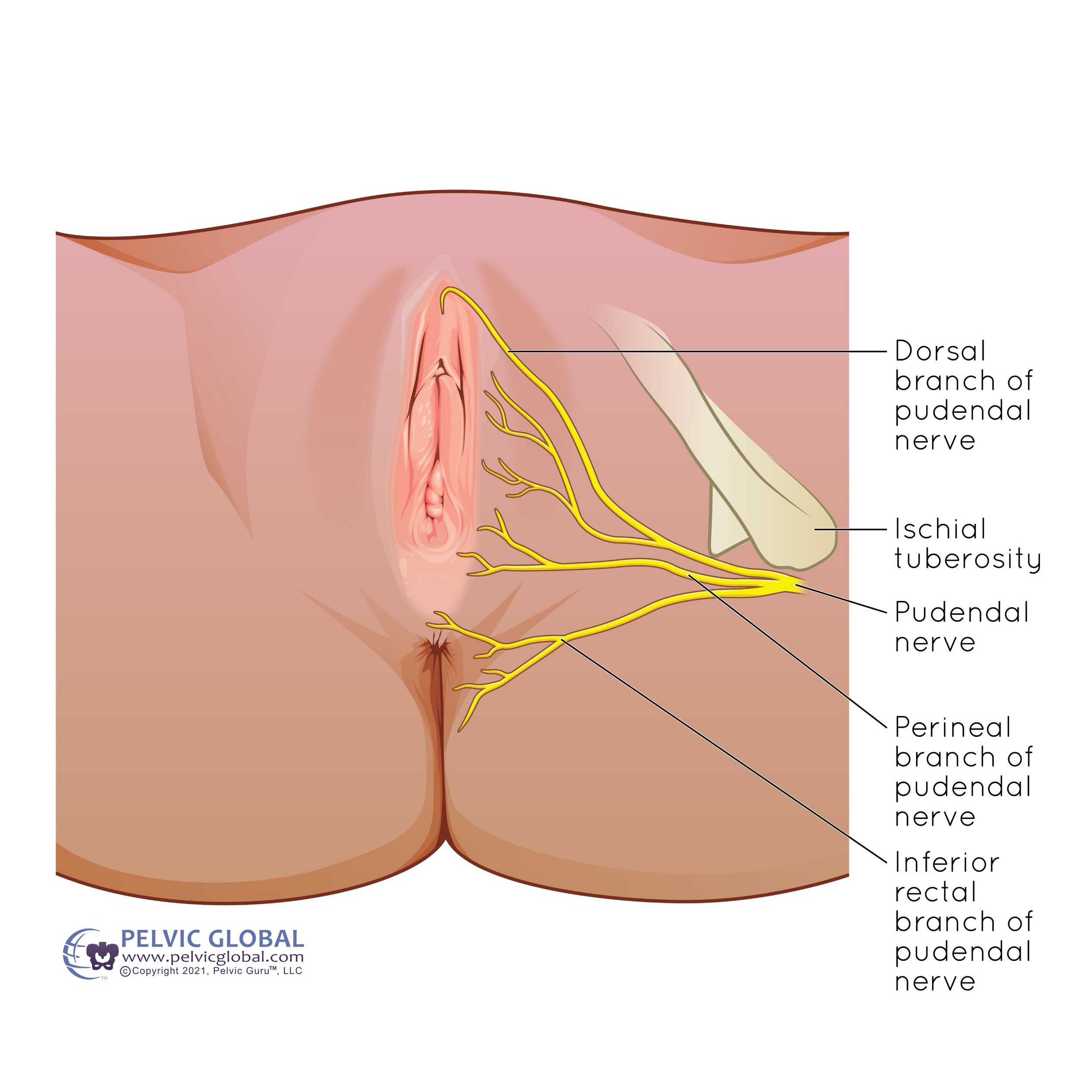
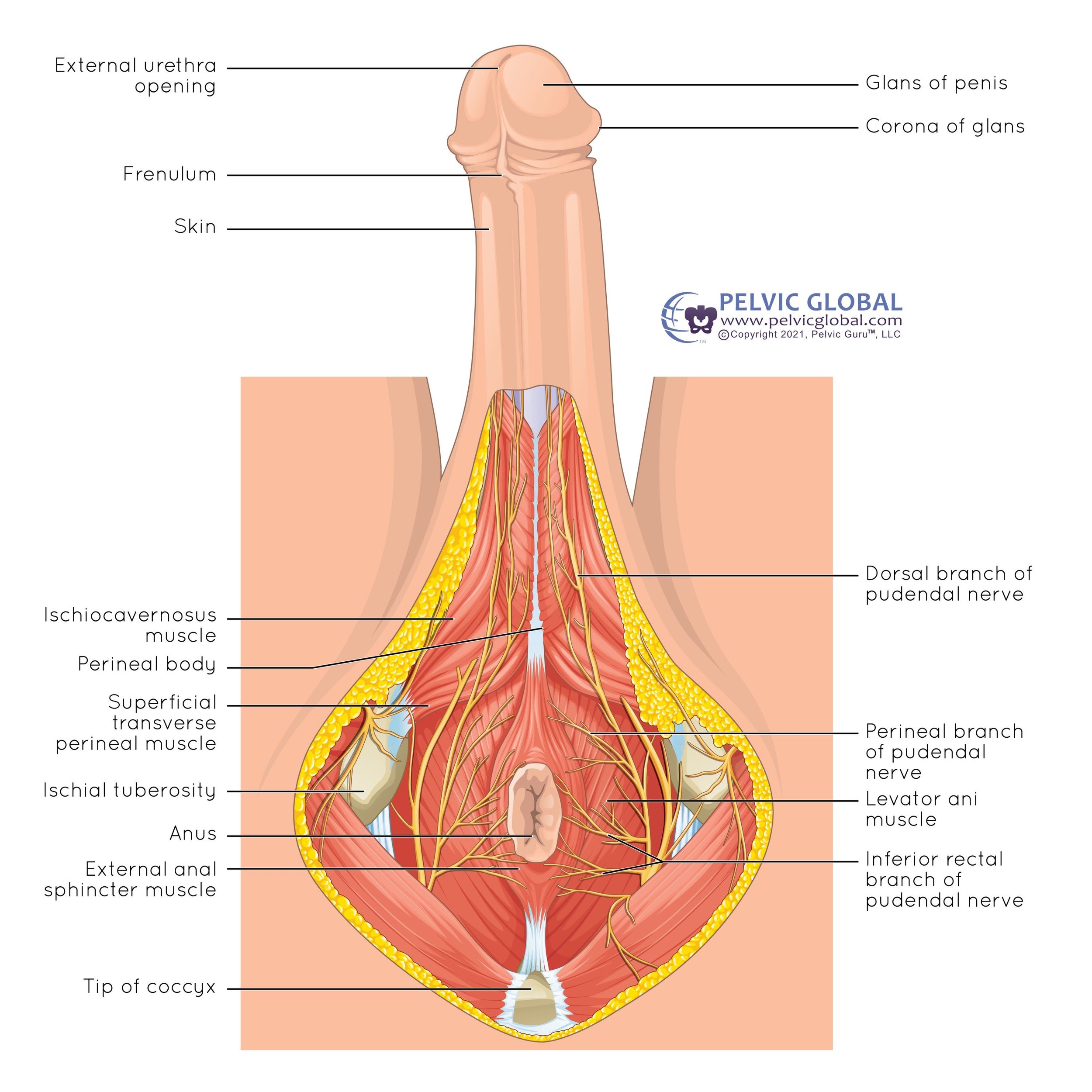
Where is the Pudendal Nerve?
The pudendal nerve is located in the pelvis. It starts from the very low back region called the sacrum, and then passes downward toward the tailbone then forward through the pelvic floor to the genital region.
What Does the Pudendal Nerve Do?
One of the roles of the pudendal nerve is to provide sensation to genitals, perineum, and anus. Its second job is to control muscles such as the pelvic floor that are responsible for urination, defecation, and sexual function.
How Common is This Condition?
Pudendal neuralgia is relatively rare, affecting an estimated 30,000 to 200,000 people in the United States. It is most common in adults over the age of 19.
Symptoms and Causes
What are the Symptoms of Pudendal Neuralgia?
The primary symptom of pudendal neuralgia is pain in the areas supplied by the pudendal nerve, such as the genitals, anus, or perineum. This pain can be:
Shooting, aching, burning, or stabbing
Aggravated by sitting
Relieved by standing, lying down, or sitting on a toilet
Located on one side of the pelvis
Other symptoms include:
Increased sensitivity, such as pain with wearing tighter clothing such as underwear, jeans, or leggings
Sensation like you are sitting on a golf ball
Urgency or frequency need to pee
Painful bowel movements or constipation
Painful sex or discmfort with arousal
Erectile dysfunction
Referred pain in the inner thigh, back of the leg, or tailbone region
What Causes Pudendal Neuralgia to Flare Up?
Pudendal neuralgia can be triggered by irritation through compression, overstretching, or microtraumas to the pudendal nerve. Common causes include:
Activities placing constant strain on the pelvic area (e.g., cycling, squatting, horseback riding)
Prolonged sitting
Chronic constipation
Direct trauma to the buttocks or back through falls
Biomechanical imbalances in the body (often with SI joint pain, back pain, or pelvic floor dysfunction).
Complications from pelvic surgeries (e.g., prostatectomy, pelvic organ prolapse repairs, or hysterectomy)
Pelvic fractures
Frequent vaginal infections
Diagnosis and Tests
How is Pudendal Neuralgia Diagnosed?
For the majority of cases pudendal neuralgia is diagnosed through dectective work of piecing together your symptoms, medical history, and a physical assessment of your body. The physical exam involves looking at the muscles and structures surrounding the pelvis, abdomen, and low back, as well as an internal assessment of your pelvic floor. Posture and how the body moves is also a huge role in providing key components to help with finding the root cause of pudendal nerve irritation.
Other testing that can help rule in pudendal nerualgia include:
Magnetic resonance imaging (MRI)
Electromyography (EMG)
Pudendal nerve terminal motor latency testing
Nerve blocks to the pudendal nerve
Similar Conditions
Pudendal neuralgia symptoms often can look like other pelvic pain conditions, which makes diagnosis difficult. These conditions such include:
Vulvodynia (pain in the vulva)
Coccydynia (tailbone pain)
Sciatica (pain from sciatic nerve irritation)
Inferior rectal nerve irritation
Management and Treatment
How is Pudendal Neuralgia Treated?
Treatment options for pudendal neuralgia include pelvic health physical therapy, medication, lifestyle changes, nerve blocks, and sometimes surgery.
Physical Therapy, Pelvic Floor
A pelvic floor physical therapist can teach exercises to relax or stretch muscles affecting the pudendal nerve. They can also perform internal pelvic floor release work to help reduce irritation to the nerve. The most important and influential role of pelvic floor therapists, is connecting your pelvic floor to the rest of your body. For instance, your posture, or certain muscle imbalances could be the reason why your symptoms arose in the first place. Working on these root causes is what will ensure that your pain stays away long term.
Lifestyle Changes
Temporarily avoiding activities that exacerbate the pain, such as prolonged sitting, cycling, squatting, or straining during bowel movements, can help manage symptoms while undergoing treatment from a pelvic floor therapist. Using a donut-shaped pillow when sitting can alleviate pressure on the pelvic floor.
Nerve Block
Pudendal nerve blocks not only are used in the diagnosis of pudendal neuralgia, but also can provide some relief of the nerve pain.
Medication
Pain relief can be achieved with painkillers or nerve stabilizing medications like gabapentin, duloxetine, amitriptyline.
Surgery
Surgery, such as pudendal nerve decompression, involves removing muscle or tissue compressing the pudendal nerve. Nerve entrapment can only be confirmed during surgery and pain relief from surgery can take months or years to achieve, thus these surgeries are usually a last resort and should be approached with caution.
FAQs About Pudendal Neuralgia and Pelvic Floor PT
Can pelvic floor physical therapy help with pudendal neuralgia?
Yes, pelvic floor physical therapy can alleviate symptoms by relaxing and stretching the muscles causing the pudendal nerve to be irritated.
What should I expect during a pelvic floor PT session?
Expect a detailed evaluation, treatment and exercises that are specific to what your individual body needs, internal work to the pelvic floor muscles, and education on lifestyle changes to help relieve symptoms.
How long does it take to see improvements with pelvic floor PT?
Improvement timelines vary because everyone’s body responds differently and heals at different rates. Additionally, healing time can be influenced by comorbidities, life stressors, and length of time your symptoms have been present. Patients may notice symptom relief within a several weeks to months of consistent therapy.
Prevention
How Can I Reduce My Risk of Pudendal Neuralgia?
Being mindful of your form and posture with repetitive activities, such as cycling, alternate sitting with standing, and avoid straining during bowel movements to reduce your risk.
Outlook / Prognosis
Can Pudendal Neuralgia Be Cured?
Pudendal neuralgia is a chronic pain condition, and because the causes and symptoms vary greatly from person to person, it is challenging to say if it can be fully cured. However, early treatment involving a multidisciplinary team can greatly help in minimizing and managing symptoms, improving the quality of life.
Living With Pudendal Neuralgia
How Do I Manage Daily Life with Pudendal Nerve Pain?
Managing daily life with pudendal nerve pain involves seeking help from the a multidisciplinary team of healthcare providers, avoiding or adjusting aggravating activities, and following through with recommended treatment plans to reduce nerve irritation.
While pudendal neuralgia can be distressing, there are plenty of options to get your back to living your life. Don’t give up hope on finding the right healthcare team and treatment plan that works for you. If you have any questions don’t hestitate to reach out to us. We’re here to help guide you on your healing journey.
Watch Dr Jana Richardson explain Pudendal Neuralgia on IG!
Written by:
Dr. Jana Richardson, PT, DPT, WCS, PRPC, CIDN
Dual Board Certified Pelvic Floor Therapist and Owner of Chicago Pelvic Health
Dr. Jana Richardson is a highly accomplished pelvic floor therapist with dual board certifications and extensive experience in treating complex pelvic floor dysfunctions. As the owner of Chicago Pelvic Health, Dr. Richardson is dedicated to providing personalized and effective care for her patients. With a Doctorate in Physical Therapy, and specialized certifications in Women’s Health and Pelvic Rehabilitation, Dr. Richardson is a leading expert in her field. She is also certified in Integrative Dry Needling, further enhancing her ability to offer comprehensive treatment plans. Dr. Richardson’s commitment to patient-centered care and her passion for helping individuals achieve optimal pelvic health make her an invaluable asset to the community.
Contact Information