Lower Crossed Syndrome and Pelvic Floor Health: How Pelvic PT Can Help
Introduction
Lower Crossed Syndrome (LCS), commonly referred to as Pelvic Crossed Syndrome (PCS), is a condition characterized by muscular imbalances around the pelvis and lower back. These imbalances can lead to chronic pain, poor posture, and other complications. This blog will explore how PCS relates to pelvic floor dysfunction and why pelvic physical therapy is the most effective treatment.
What is Pelvic Crossed Syndrome?
Lower Crossed Syndrome involves muscle imbalances where certain muscles, such as the hip flexors and lumbar extensors, are overly tight, while others, like the abdominals, hamstrings, and gluteal muscles, are weak. This imbalance creates a “cross” pattern, leading to an anterior pelvic tilt, increased lumbar lordosis (or increased low back curve), and compensatory postural imbalances.
Key findings: Anterior pelvic tilt, increased lower back curvature, tight hip flexors, weak glutes, hamstrings, and abdominals, lower back pain, lower belly pooch.
Clinical Presentation: Individuals with PCS often experience joint dysfunction, pain in the lower back, hip, and knees, and a characteristic swayback posture. Tight hip flexors and weak abdominals and gluteal muscles contribute significantly to these imbalances.
Anatomy of Lower Crossed Syndrome:
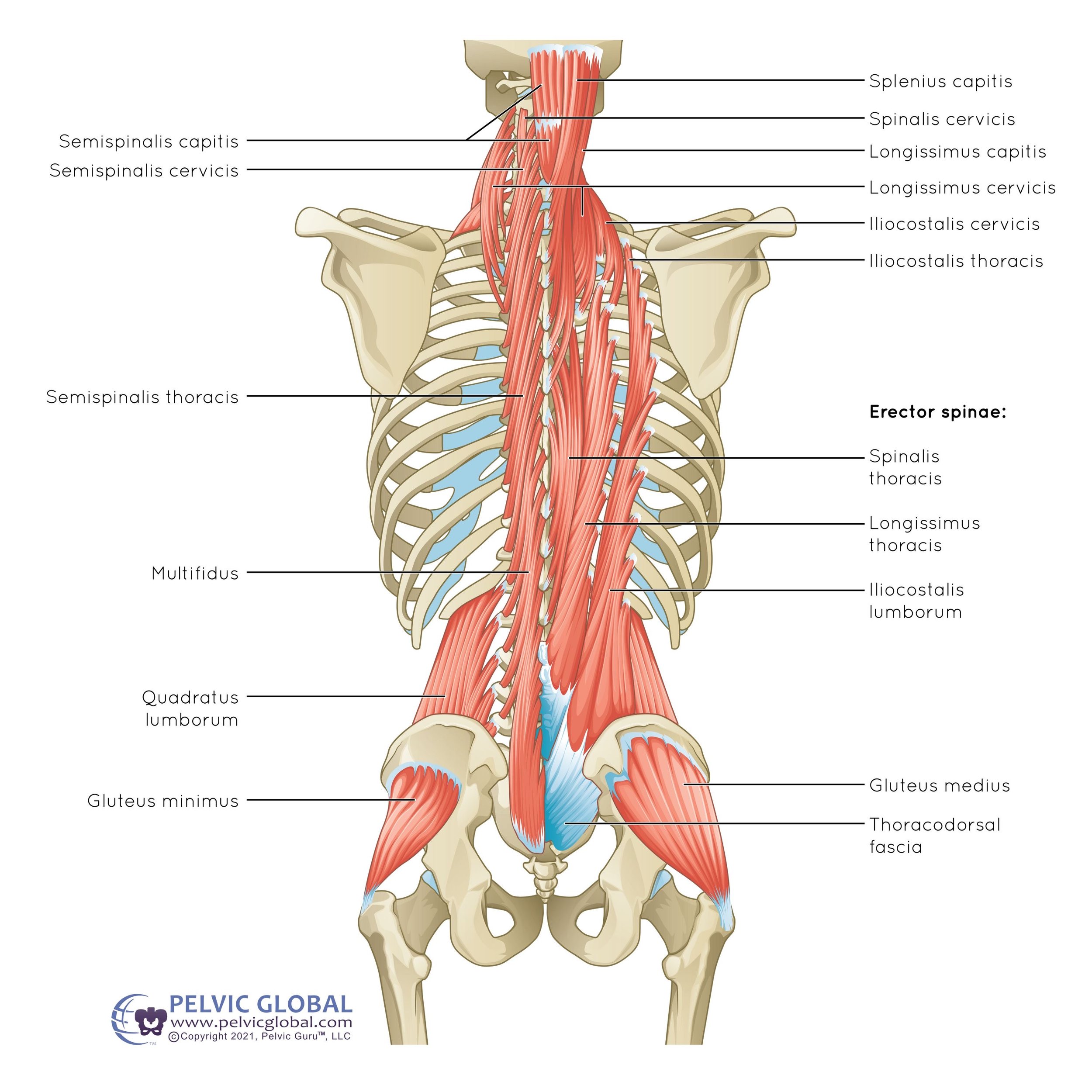
This image illustrates some of the key muscles involved in Lower Crossed Syndrome (LCS), including the low back muscles (erector spinae, quadratus lumborum) and gluteal muscles (gluteus medius, and minimus.) Imbalances in these muscles, such as tightness in the lower back muscles and weakness in the glutes, are common in LCS and can lead to lower back pain and posture issues.
Top Reasons Someone Might Develop Lower Crossed Syndrome (LCS)
1. Sedentary Lifestyle & Poor Posture
Sitting for long periods—whether in front of a computer, at school, or watching TV—can cause muscle imbalances. The hip flexors stay in a shortened position which can make them tight, while the glutes stay in a lengthened position which can lead to weakness over time and lead to Lower Crossed Syndrome (LCS). Furthermore poor posture in these prolonged seated positions, such as slouching can further worsen this.
Real-World Example: A person who has a desk job who sits all day at a computer and then sits again for a long drive home may be prone to develop tight hip flexors and weak glutes, especially if not counteracting these positions by stretching or strengthening the right muscles.
2. Unbalanced Workouts & Muscle Weakness
Focusing on certain muscle groups while neglecting others can result in imbalances. Overworking muscles like the hip flexors and lower back without strengthening the core and glutes can lead to LCS. Some people naturally have weaker muscles in these areas, which exacerbates the issue.
Real-World Example: A gym-goer who frequently performs squats but skips core exercises or someone who doesn’t exercise regularly might experience lower back pain due to imbalances between muscle groups.
3. Injuries, Chronic Pain, & Age-Related Changes
Injuries to the lower back or hips, chronic pain, and age-related muscle loss can all contribute to LCS. These factors often result in altered movement patterns, tight muscles, and weakening of core muscles, leading to imbalances.
Real-World Example: An individual who suffered a back injury or an older adult with decreased activity levels may experience more lower back pain and tightness due to weakened muscles and poor movement patterns.
4. Repetitive Movements or Job-Related Risks
Jobs that require the same movements repeatedly or involve long periods of sitting or standing can lead to muscle imbalances. Repeated bending, lifting, or poor posture at work can strain the lower back and pelvic muscles.
Real-World Example: A person who frequently bends over to lift heavy objects without proper technique might strain their lower back and develop LCS. Similarly, a driver who spends long hours seated could develop tight hip flexors and weak glutes from prolonged positioning.
5. Genetic Factors
Some people may be more likely to develop muscle imbalances due to their genetics. For example, they might naturally have a more pronounced curve in their lower back or a tendency for their pelvis to tilt forward.
Real-World Example: A person whose parents have a similar body posture or muscle imbalance might also experience the same issues, making them more prone to to LCS if not managed with proper exercises.
6. Poor Ergonomics at Work or Home
Having a poorly set up workspace can greatly affect your posture and muscle tension. If your desk, chair, or even the way you sit at work or home isn’t properly adjusted, it can lead to strains that contribute to LCS.
Real-World Example: A person working from home without an ergonomic chair or an ergonomic set up might sit in a slouched position all day, causing tightness in the lower back and weakening the abdominal muscles, which can lead to LCS.
How LCS Affects the Pelvic Floor
The pelvic floor muscles play a crucial role in stabilizing the pelvis and supporting your back and core system. When there is an imbalance in the muscles associated with LCS, the pelvic floor can become either overly tense or weak. This can lead to symptoms such as:
Lower Crossed Syndrome (LCS) Explained:
This image illustrates the muscle imbalances in Lower Crossed Syndrome, where tight hip flexors and lower back muscles combine with weak gluteal and abdominal muscles. These imbalances result in an anterior pelvic tilt, leading to poor posture and potential lower back pain. Pelvic physical therapy can help restore balance and correct posture.
Why Pelvic Physical Therapy is the Best Treatment Option
Pelvic physical therapy is highly effective for managing LCS due to its focus on connecting what is happening at the pelvic floor muscles to the core system and overall posture. Pelvic PT focuses on:
Muscle Strengthening and Stretching: Exercises that target commonly weak muscles (e.g., abdominals, gluteals) and stretch tight muscles (e.g., hip flexors, lumbar extensors) can restore balance and proper alignment.
Postural Retraining and Ergonomics: By looking at what your body is doing with various activities can help to ensure that you aren’t compensating or overworking certain muscles in a way that would contribute to muscle imbalances.
Myofascial Release Work: These techniques help relieve muscle tension, improve flexibility, and allow your deep core system to work as they were naturally designed.
Breathing and Core Stabilization Exercises: Training patients on proper breathing techniques helps with core stability thus helping to support the pelvic floor muscles.
Research Evidence Supporting Pelvic PT for LCS/PCS
Research indicates that targeted stretching and strengthening exercises improve muscle balance and reduce symptoms associated with PCS. A study involving children with PCS demonstrated significant improvement in muscle strength and reduced muscle tension after a five-week exercise intervention focused on stretching the iliopsoas and strengthening the abdominal and gluteal muscles. (1)
Furthermore, studies on adults, including office workers and athletes, show that pelvic PT interventions like core stabilization, posture correction, and tailored exercise programs can reduce pain, improve posture, and enhance quality of life. (2)
Practical Tips for Managing PCS with Pelvic PT
Stay Consistent with Exercises: Regularly performing prescribed exercises is crucial for maintaining muscle balance and preventing the recurrence of PCS.
Focus on Core Strength: Incorporate exercises that target both the deep abdominal muscles and the glutes. This not only supports the pelvis but also alleviates stress on the lumbar spine.
Stretch Tight Muscles Daily: Include daily stretching of the hip flexors, hamstrings, and lumbar extensors to maintain flexibility and prevent further imbalances.
Monitor Your Posture: Awareness of your posture throughout the day, especially during prolonged sitting or standing, can help reduce stress on the pelvic and lumbar regions.
Conclusion
Lower Crossed Syndrome aka Pelvic Crossed Syndrome is a common yet often overlooked condition that significantly impacts both pelvic floor health and spinal health. Through the focused and specialized treatment techniques of pelvic physical therapy, individuals can correct muscle imbalances, improve posture, alleviate pain, and properly strengthen their core system. If you suspect you have LCS or are experiencing related symptoms, consider consulting a board-certified pelvic physical therapist for a treatment plan specific to your body’s needs.
If you're dealing with pelvic pain or suspect you might have Pelvic Crossed Syndrome, don't wait—reach out to a pelvic health specialist today. Our team at Chicago Pelvic Health is here to help you regain your balance and live pain-free.
Written By,
Dr. Jana Richardson, PT, DPT, WCS, PRPC, CIDN
Dual Board Certified Pelvic Floor Therapist and Owner of Chicago Pelvic Health
Dr. Jana Richardson is a highly accomplished pelvic floor therapist with dual board certifications and extensive experience in treating complex pelvic floor dysfunctions. As the owner of Chicago Pelvic Health, Dr. Richardson is dedicated to providing personalized and effective care for her patients. With a Doctorate in Physical Therapy, and specialized certifications in Women’s Health and Pelvic Rehabilitation, Dr. Richardson is a leading expert in her field. She is also certified in Integrative Dry Needling, further enhancing her ability to offer comprehensive treatment plans. Dr. Richardson’s commitment to patient-centered care and her passion for helping individuals achieve optimal pelvic health make her an invaluable asset to the community.
Contact Information:
References: