Top 3 Pelvic Pains Linked to Constipation—and How to Find Relief
How Constipation Causes Pelvic Pain: Top Issues and How to Get Relief
Introduction
Did you know that the discomfort of constipation can ripple far beyond your digestive tract? If you've been experiencing unexplained pelvic pain, tailbone pain, or even discomfort during sex, constipation might be the hidden culprit.
In this article, we'll delve into the top three pelvic pains linked to constipation and offer practical advice on how to address them. By recognizing these signs, you can take proactive steps to improve your well-being and regain comfort in your daily life.
1. Tailbone Pain
How Constipation Can Lead to Muscle Overactivity
Constipation is more than just having infrequent bowel movements or passing small, hard stools. It can cause significant changes in the pelvic floor muscles. When stool accumulates in the rectum, it stretches the rectal canal and exerts extra pressure on surrounding muscles, including the puborectalis. This muscle plays a big role in bowel control by helping to retain stool. If the puborectalis is constantly tasked with holding back stool, it can become overactive, leading to tailbone pain.
Understanding the Connection Between Tailbone Pain and Muscle Overactivity
The tailbone, or coccyx, is located at the bottom of the spine and functions as an anchor for several muscles, ligaments, and tendons in the pelvic area. This includes the puborectalis muscle which attaches directly to the tailbone. When the puborectalis is consistently overworked, it can pull on the tailbone, leading to discomfort and pain. This ultimately can also lead to a cyclical pattern where tailbone pain makes it even more difficult to pass stools.
Female Pelvis
This image shows the function of the puborectalis muscle in a female. One of it’s roles is in bowel control. When stool is backed up it, it can cause this muscle to overwork and thus pull on the tailbone resulting in tailbone pain.
Male Pelvis
This image shows a similar view of the pelvic floor muscles in a male. The puborectalis muscle located at the bottom by the rectal canal.
2. Pudendal Neuralgia: A Stretch Injury
Another condition linked to constipation-induced pelvic pain is pudendal neuralgia. The pudendal nerve runs through your pelvis close to the rectum and is responsible for sensations in the pelvic region. Constipation can irritate this nerve leading to pudendal neuralgia symptoms:
Sharp or Burning Pain: Often felt in “saddle” region around the genitals, perineum, or rectal area.
Increased Discomfort When Sitting: Sitting may exacerbate the pain due to pressure on the nerve. However sitting on a toilet seat may not be bothersome.
Bladder Changes: You might feel increased urinary urgency, urinary frequency, or feeling like you have a UTI.
Where is the Pudendal Nerve?
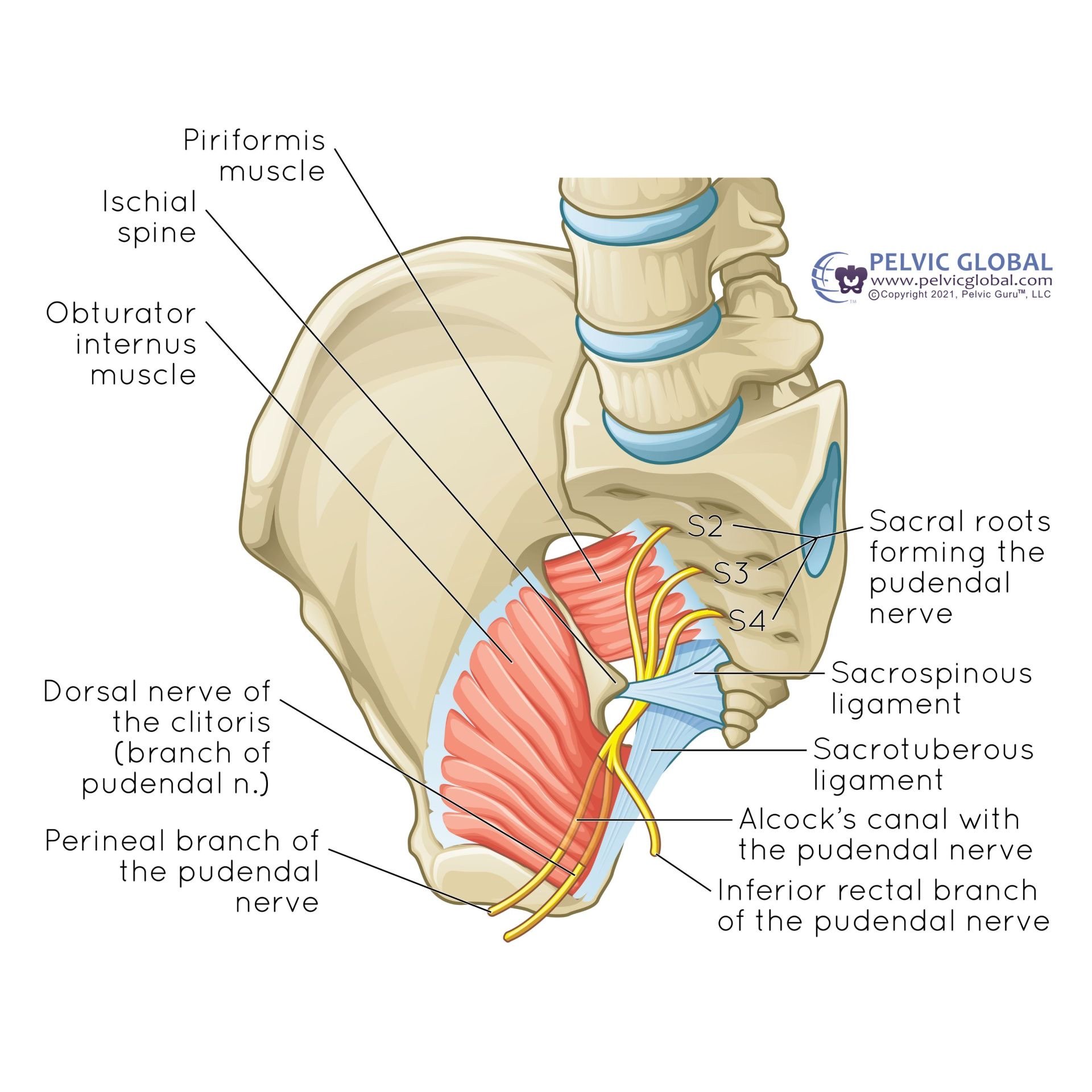
Pudendal Nerve
The pudendal nerve, shown here, runs through the pelvic region. It can become irritated by straining, or the over stretching of the rectal canal during constipation.
Why Does This Happen?
Neural Stretch: Chronic straining during bowel movements can stretch the nerve by pulling its pathway as it moves through the pelvis.
Nerve Compression: The buildup of stool and straining can put extra pressure the pudendal nerve causing irritation.
Muscle Overactivity: Tight pelvic floor muscles can put additional pressure on the nerve.
3. Painful Sex
The Unexpected Impact on Intimacy
Constipation can affect your sex life in surprising ways. A full rectum presses against the vaginal canal, reducing its ability to stretch during intercourse. This pressure can cause discomfort or pain, making intimacy less enjoyable.
Understanding the Connection
Physical Pressure: The accumulated stool in the rectum physically encroaches on vaginal space.
Muscle Tension: Overactive pelvic floor muscles, irritated from constipation, can tighten during sex.
Decreased Lubrication: Stress and discomfort can reduce natural lubrication, exacerbating pain.
Understanding the Bigger Picture
Constipation is more than a minor inconvenience; it's a condition that can significantly impact your quality of life. By recognizing the connection between constipation and pelvic pains—including conditions like pudendal neuralgia—you can take proactive steps to address the root cause.
Tips for Managing Constipation
Dietary Changes: Increase your fiber intake with fruits, vegetables, and whole grains to promote regular bowel movements. A diet rich in fiber helps with good stool formation.
Stay Hydrated: Drinking plenty of water softens stool, making it easier to pass and reducing straining.
Proper Toilet Posture: Using a small stool, like a Squatty Potty, to elevate your feet can align your rectum more naturally, and allows for more complete emptying.
Regular Exercise: Physical activity, even as simple as walking helps to stimulate our bowels to move. Just like we walk our animals to poop, we should walk ourselves too.
Daily routine: Bowels like routine and work off your circadian rhythm. Trying to get up and go to sleep around similar times helps to establish this.
Eating all meals: Eating and chewing helps to stimulate our natural emptying reflex, the gastrocolic reflex.
Relaxation techniques: Stimulating our relaxing nervous system, the parasympathetic nervous system, helps to allow our body to “rest and digest”. Doing things like diaphragm breathing can help to tap into this part of your nervous system.
Heat: a warm heating pad to the abdomen, or drinking something warm can help to stimulate your bowels to move.
When to See a Healthcare Professional
If you experience persistent pelvic pain, painful sex, or tailbone pain, it's essential to consult a healthcare provider. These symptoms can be signs of underlying conditions that require medical attention.
Conclusion
Constipation's effects extend beyond the bathroom, influencing various aspects of your health and well-being. By understanding how it contributes to pelvic pain —including conditions like pudendal neuralgia—painful sex, and tailbone pain, you can take steps to alleviate these discomforts.
Don't let constipation control your life. Implement the strategies discussed, and consider reaching out to a Board Certified pelvic floor physical therapist for personalized guidance. Your journey to improved pelvic health starts here.
Ready to find relief? Contact Chicago Pelvic Health & Wellness today to schedule a consultation with our experienced pelvic floor therapists. We're here to help you navigate your path to better health.
Written By,
Dr. Jana Richardson, PT, DPT, WCS, PRPC, CIDN
Dual Board Certified Pelvic Floor Therapist and Owner of Chicago Pelvic Health
Dr. Jana Richardson is a highly accomplished pelvic floor therapist with dual board certifications and extensive experience in treating complex pelvic floor dysfunctions. As the owner of Chicago Pelvic Health, Dr. Richardson is dedicated to providing personalized and effective care for her patients. With a Doctorate in Physical Therapy, and specialized certifications in Women’s Health and Pelvic Rehabilitation, Dr. Richardson is a leading expert in her field. She is also certified in Integrative Dry Needling, further enhancing her ability to offer comprehensive treatment plans. Dr. Richardson’s commitment to patient-centered care and her passion for helping individuals achieve optimal pelvic health make her an invaluable asset to the community.









Are you noticing thinner stools and wondering if something’s amiss? Uncover how pelvic floor dysfunction can play a role and explore practical ways to address it. Written by a dual board-certified Pelvic PT, this guide offers insight, reassurance, and clear steps toward improving bowel health.